John Dyben, DHSc | Chief of Research and Innovation
A downloadable PDF of the white paper is available here.
A Preliminary Examination of the Efficacy of Brainspotting with Patients in Residential Treatment for Substance Use Disorders and Co-occurring Trauma Related Disorders
Trauma and Substance Use Disorders
The scientific and treatment community has long known that there is a correlation between trauma and substance use disorders (SUD) with a comingling pathology wherein each complicates the other in a synergy of distress (Levin et al, 2021; Najavits et al, 2020). How this relationship works is not fully understood. What is certain, however, is that competent treatment of SUD necessarily includes the treatment of trauma related disorders (TRD) and vice versa.
Brainspotting
Brainspotting (BSP) is a neurophysiological psychotherapeutic approach aimed at improving symptoms resulting from TRD including anxiety, mood dysregulation, hypervigilance and others (Mason & Moukouta, 2017). This approach is an elaboration on Eye Movement Desensitization and Reprocessing (EMDR) and Somatic Experiencing (SE) and involves an emotionally and somatically focused clinical interview while patients follow the therapist’s fingers or other object. Particular points in the patient’s field of vision are identified as “Brainspots,” which are understood to be areas that can connect to unprocessed trauma so that the trauma be accessed and treated (D’Antoni et al, 2022; Hildebrand et al, 2017).
A relatively new psychotherapy, BSP was developed in 2003 by Licensed Clinical Social Worker, David Grand, PhD (Corrigan et al, 2015). Given the relative newness of this approach, the number of studies and articles produced on the topic are limited. However, the literature that presently exists consists of a growing body of evidence suggesting that BSP provides relief from symptoms in participants.
Hildebrand et al (2017) completed a multicenter, multinational longitudinal study comparing the efficacy of BSP to that of EMDR in the reduction of Post-traumatic Stress Disorder (PTSD) symptoms as well as depression and anxiety. 76 clients participated in the study, and clients self-selected to be treated with three sessions of either EMDR (n=23) or BSP (n=53). Clients who chose BSP were given the optionto receive EMDR if they were not satisfied with BSP. No clients chose this option. Clients completed self-report measures prior to the first session, one week after the third session, and around six months after treatment. Both groups reported significant improvement in symptoms. The BSP group had smaller effect sizes, but there was no significant difference in outcomes.
D’Antoni (2021) utilized both subjective (self-report scales) and objective (Heart Rate [HR] and Heart Rate Variability [HRV]) measures to compare the effects of BSP compared to a control of Body Scan Meditation (BSM). Subjects (N=28) were exposed to BSP and BSM in a randomized order. The results of this study found a greater improvement in self-reported symptoms as well as increased calm and relaxation in the BSP group as interpreted by changes in HR and HRV measures.
Recently, D’Antoni et al (2022) published a study comparing the effects of BSP, EMDR, and BSM on self-report symptoms of distress, with a control intervention of book reading (BR). The subjects were psychologists (n=37) and medical doctors (n=3). Participants received one session of each intervention, including the control. Consistent with other research, this group found BSP and EMDR to demonstrate similar efficacy in decreasing distressing symptoms.
As of the writing of this paper, this writer has not found any study that challenges the findings of the above-mentioned studies, which indicate that BSP is an effective tool for improving symptoms of post-traumatic stress.
Population
To date, there does not appear to be any study of the efficacy of BSP within a population of individuals who have both symptoms of TRD and co-occurring substance use disorders (SUD). Hanley Foundation (HF) provides treatment for this population in both residential and non-residential levels of care and is committed to measuring the efficacy of interventions with patients and to do so with special attention when utilizing a technique for which there is not a foundation of evidence with the specific TRD/SUD population.
Patients participating in this examination of efficacy (EOE) were in a residential level of care in a HF program.
Methods
Results
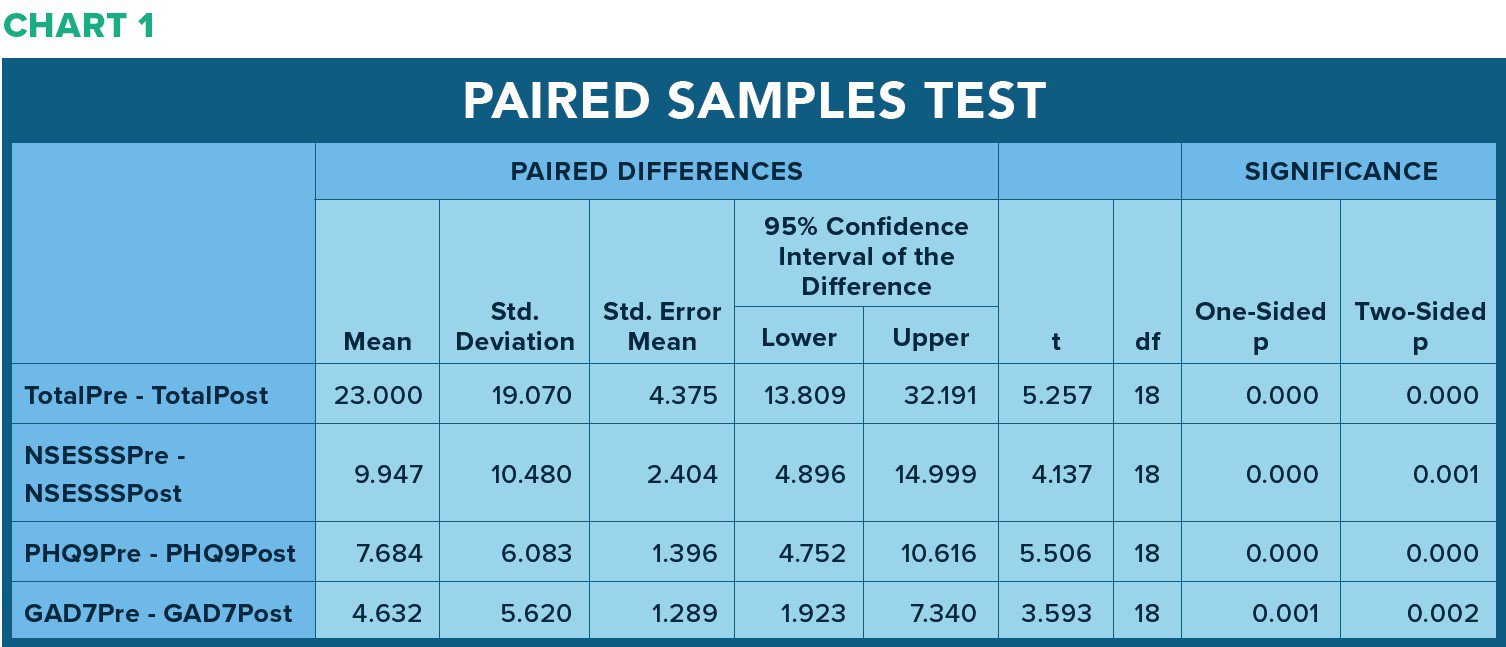
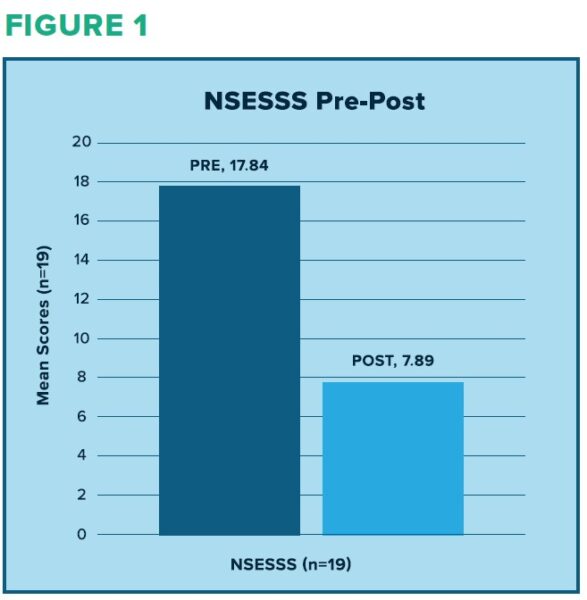
NSESSS scores measuring severity of symptoms related to traumatic stress decreased from a mean of 17.84 to a mean of 7.89, a 44% decrease (Figure 1).
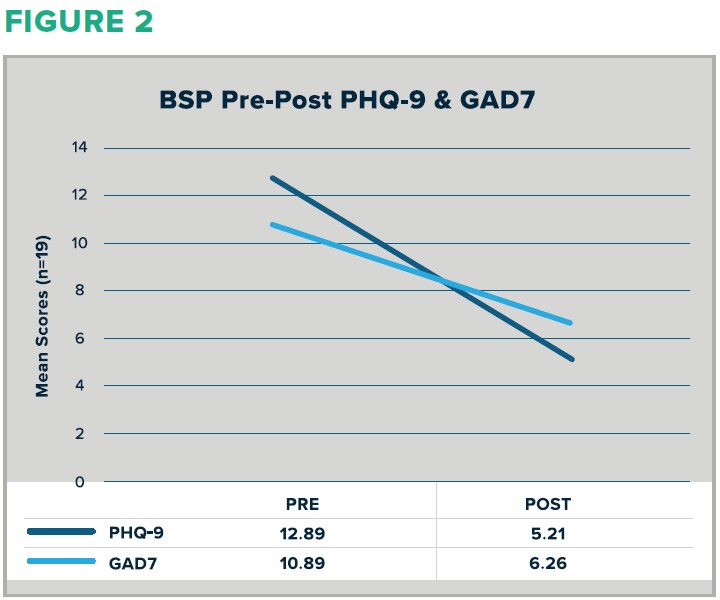
PHQ-9 scores measuring depression decreased from a mean of 12.89 to a mean of 5.21, a 40% decrease (Figure 3).
GAD-7 scores measuring anxiety decreased from a mean of 10.89 to a mean of 6.26, a 57% decrease (Figure 3).
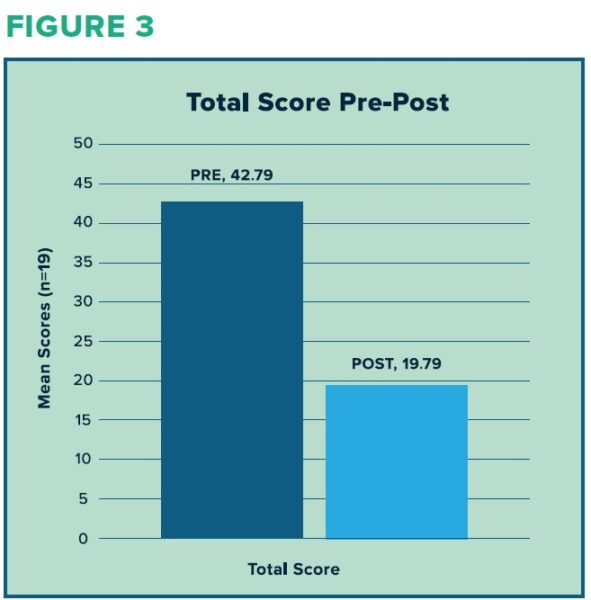
Combined scores (sum of NSESSS, PHQ-9, and GAD-7 scores) decreased from a mean of 42.79 to a mean of 19.79, a 46% decrease (Figure 2).
BSP compared to TAU PHQ-9 and GAD-7 scores:
A one-way analysis of variance (ANOVA) was used to compare differences in PHQ-9 and GAD-7 scores between patients who completed a session of BSP and those who received TAU. In the comparison of these groups, there was a statistically significant difference between the groups on the PHQ-9 scores though not on the GAD-7 scores (see Chart 2).
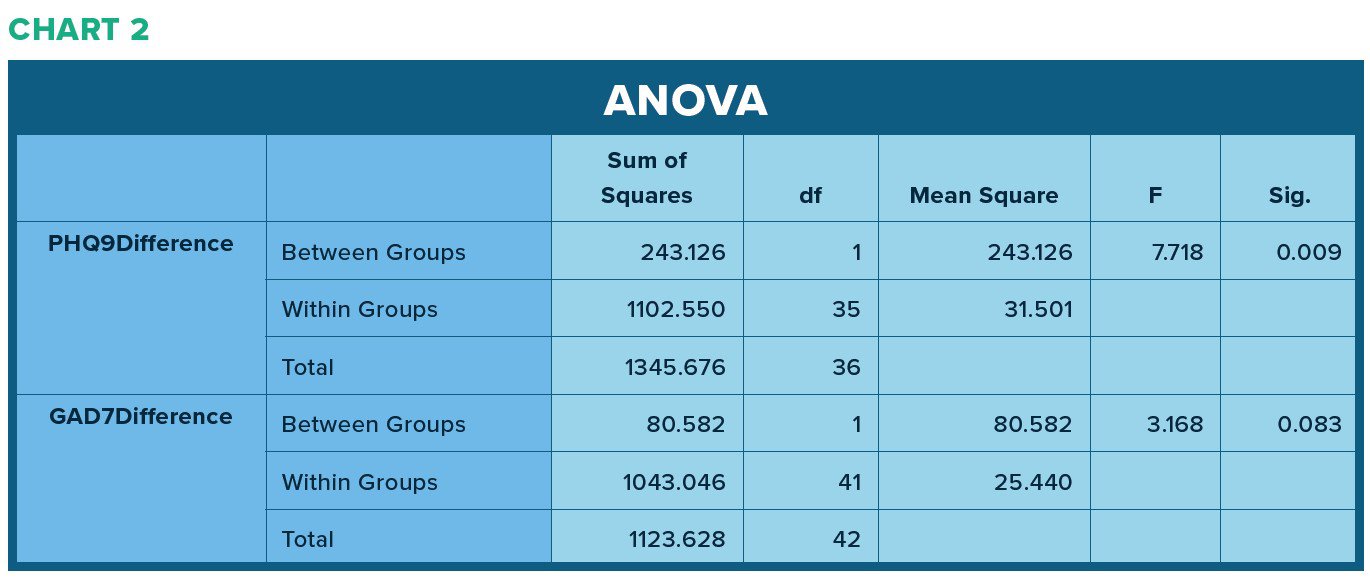
The mean scores for the TAU group baseline test (PHQ-9 = 7.11; GAD-7 = 7.13) is substantially lower than the baseline (pre) scores for the BSP group (PHQ-9 = 12.89; GAD& = 10.89). This may indicate an unidentified confounder.
Discussion
The evidence from this preliminary investigation indicates that BSP is effective in decreasing symptoms related to trauma, depression, and anxiety. In comparison to a group within the same cohort, BSP appears to have a greater effect on decreasing symptoms of depression as measured in the PHQ-9 over TAU, though this should be considered an area for further investigation rather than a conclusive finding at this time. Data gathered from this internal EOE provides support for the use of Brainspotting to decrease symptoms related to trauma, depression, and anxiety with patients in residential treatment for co-occurring SUD and post-traumatic stress.
There are limitations to these findings. In addition to a small BSP sample size and potential confounding factors between BSP and TAU groups, variables including age, gender, and specific diagnoses are not accounted for. Further investigation of the efficacy and utility of BPS with this population is warranted.
References
Corrigan, F. M., Grand, D., & Raju, R. (2015). Brainspotting: Sustained attention, spinothalamic tracts,
thalamocortical processing, and the healing of adaptive orientation truncated by traumatic
experience. Medical Hypotheses, 84(4), 384–394.
D’Antoni, F. (2021). Brainspotting reduces disturbance and increases Heart Rate Variability linked to
distressing memories: A pilot study. Mediterranean Journal of Clinical Psychology, 9(3).
D’Antoni, F., Matiz, A., Fabbro, F., & Crescentini, C. (2022). Psychotherapeutic Techniques for
Distressing Memories: A Comparative Study between EMDR, Brainspotting, and Body
Scan Meditation. International Journal of Environmental Research and Public Health, 19(3).
Hildebrand, A., Grand, D., Stemmler, M. (2017). Brainspotting – the efficacy of a new therapy
approach for the treatment of Posttraumatic Stress Disorder in comparison to Eye
Movement Desensitization and Reprocessing. Mediterranean Journal of Clinical
Psychology, 5(1).
Levin, Y., Lev Bar-Or, R., Forer, R., Vaserman, M., Kor, A., & Lev-Ran, S. (2021). The association
between type of trauma, level of exposure and addiction. Addictive Behaviors, 118.
Masson, J., Bernoussi, A., & Moukouta, C. S. (2017). Brainspotting therapy: About a Bataclan
victim. Global Journal of Health Science, 9(7), 103.
Najavits, L. M., Clark, H. W., DiClemente, C. C., Potenza, M. N., Shaffer, H. J., Sorensen, J. L., Tull,
M. T., Zweben, A., & Zweben, J. E. (2020). PTSD/Substance Use Disorder Comorbidity:
Treatment Options and Public Health Needs. Current Treatment Options in Psychiatry,
7(4), 544–558.
Palsimon Jr, T. O. (2022). The preliminary efficacy and clinical applicability of Brainspotting
among Filipino women with severe posttraumatic stress disorder. Archives of Psychiatry &
Psychotherapy, 24(1), 54–64.